Exploring the Role of Electronic Health Record (EHR) Systems in Improving Medical Practice7/26/2023 Electronic Health Record (EHR) systems have revolutionized the healthcare industry by transforming the way medical information is stored, accessed, and shared. These digital platforms allow healthcare providers to maintain comprehensive and real-time patient records, leading to improved medical practice and patient care.
One of the significant advantages of EHR systems is the centralized access to patient data. Healthcare professionals can quickly retrieve patient history, medication records, lab results, and treatment plans, enabling better-informed decision-making. This enhanced accessibility promotes coordinated care and reduces the risk of medical errors, resulting in improved patient outcomes. Moreover, EHR systems streamline administrative tasks, reducing paperwork and manual documentation. This efficiency allows healthcare providers to spend more time with patients, strengthening doctor-patient relationships and enhancing patient satisfaction. Additionally, EHR systems facilitate seamless communication and information exchange among healthcare providers, specialists, and laboratories. This interoperability promotes care coordination, especially in complex cases where multiple specialists are involved in a patient's treatment. Due to the expanding use of electronic health records, or EHR, and the acceptance of healthcare IT solutions, the global Electronic Health Record (EHR) Systems Market is expanding rapidly. Furthermore, EHR systems support evidence-based medicine and research by enabling the collection and analysis of large-scale healthcare data. Healthcare organizations can use anonymized data to identify trends, patterns, and treatment outcomes, ultimately contributing to medical advancements and healthcare improvements. EHR systems play a pivotal role in improving medical practice by providing comprehensive patient data, streamlining administrative tasks, facilitating care coordination, and promoting evidence-based medicine. As technology continues to advance, the integration of artificial intelligence and predictive analytics in Electronic Health Record (EHR) Systems holds the potential to further enhance medical decision-making and patient care in the future.
0 Comments
Cervical abnormalities and the risk of cervical cancer pose significant health concerns for women worldwide. However, with advancements in medical technology, there are now more effective methods of early detection and prevention. One such method that has revolutionized the field is Colposcope. This diagnostic procedure offers numerous benefits in identifying and managing cervical abnormalities, providing women with a higher chance of successful treatment and improved health outcomes.
Colposcopic is a visual examination of the cervix using a colposcopic, a magnifying instrument that provides an enhanced view of the cervical tissue. It is typically recommended when an abnormal Pap smear or HPV test result is obtained, indicating the presence of potentially pre-cancerous or cancerous cells. By allowing clinicians to closely examine the cervix, colposcopic enables them to identify abnormal areas that may not be visible to the naked eye, leading to more accurate diagnoses and tailored treatment plans. One of the primary advantages of colposcopic is its ability to detect and differentiate between high-grade and low-grade lesions. This differentiation is crucial in determining the appropriate course of action. High-grade lesions are more likely to progress to cervical cancer if left untreated, while low-grade lesions may resolve on their own. Through Colposcope, healthcare providers can obtain targeted biopsies of suspicious areas, allowing for precise diagnosis and treatment decisions. By identifying high-grade lesions early on, women can receive timely interventions, preventing the development of cervical cancer. Moreover, colposcopic provides an opportunity for directed therapy during the same procedure. If abnormal areas are identified, various treatment modalities can be employed, such as cryotherapy or loop electrosurgical excision procedure (LEEP). These techniques involve removing or destroying the abnormal tissue, reducing the risk of progression to cancer. This immediate intervention not only offers convenience to patients but also reduces the need for multiple appointments and potential delays in treatment. Colposcope also plays a crucial role in follow-up care after treatment for cervical abnormalities. It allows healthcare providers to monitor the healing process and assess the success of the intervention. Regular colposcopic examinations post-treatment enable the detection of recurrent abnormalities or new lesions, facilitating prompt intervention and minimizing the risk of cancer recurrence. This comprehensive approach ensures that women receive ongoing surveillance and appropriate care, enhancing their long-term well-being. Additionally, colposcopic can provide reassurance to patients with normal or low-grade findings, alleviating anxiety and offering peace of mind. It allows healthcare providers to confirm the absence of significant abnormalities or provide further guidance on managing low-grade lesions. The detailed visual examination and expert interpretation offered by colposcopic instill confidence in the accuracy of the results, enhancing patient satisfaction and trust in their healthcare provider. It is important to note that Colposcope is a safe procedure with minimal risks and complications. While some women may experience mild discomfort during the examination, complications are rare. The benefits of early detection and targeted treatment far outweigh the potential discomfort associated with the procedure. Healthcare providers are skilled in ensuring patient comfort and explaining the process, further reducing any apprehension. Colposcopic is a vital tool in the early detection and management of cervical abnormalities. By providing an enhanced visualization of the cervix and targeted biopsies, it enables precise diagnoses and treatment decisions. The ability to perform directed therapy during the same procedure and monitor post-treatment care ensures comprehensive and timely interventions. Moreover, colposcopic offers reassurance to patients with normal or low-grade findings while minimizing the risk of missing high-grade lesions. With its numerous benefits, Colposcope plays a pivotal role in safeguarding women's health by detecting cervical abnormalities and preventing the progression to cervical cancer. Oxygen therapy plays a vital role in the treatment of various respiratory conditions and has proven to be a life-saving intervention for patients suffering from chronic obstructive pulmonary disease (COPD), asthma, pneumonia, and other respiratory ailments.
Traditionally, oxygen therapy involved the use of standard oxygen tanks or cylinders, but with advancements in medical technology, personalized treatment options are now available through the use of Medical Oxygen Concentrators. These innovative devices have revolutionized the way oxygen therapy is delivered, providing a range of benefits for patients and healthcare providers alike. Oxygen generators are compact and portable devices designed to extract oxygen from the surrounding air and deliver it to the patient at a consistent flow rate. Unlike traditional oxygen cylinders that require regular refilling, concentrators generate oxygen on-demand, eliminating the need for cumbersome deliveries and reducing costs in the long run. This convenience allows patients to lead more active and independent lives, without the constraints imposed by traditional oxygen therapy. One of the key advantages of Medical Oxygen Concentrators is their ability to provide customized treatment. Each patient's oxygen therapy needs may vary based on their condition, activity level, and overall health. With concentrators, healthcare providers can easily adjust the flow rate and oxygen concentration to suit individual requirements. This personalized approach ensures that patients receive the precise amount of oxygen they need, promoting optimal therapeutic outcomes and enhancing their quality of life. Furthermore, oxygen generators offer versatility in terms of delivery methods. They can deliver oxygen through various interfaces, including nasal cannulas, masks, and even specialized devices for pediatric patients. This flexibility allows healthcare providers to tailor the treatment to the patient's comfort and convenience, ensuring compliance and adherence to therapy. By offering a range of delivery options, concentrators make oxygen therapy more accessible and manageable for patients of all ages. Another significant benefit of Medical Oxygen Concentrators is their energy efficiency and eco-friendliness. Unlike traditional oxygen cylinders that require continuous refilling, concentrators draw in ambient air, extract oxygen, and deliver it directly to the patient. This process significantly reduces energy consumption and minimizes the carbon footprint associated with oxygen therapy. By opting for concentrators, healthcare facilities can contribute to environmental sustainability while providing high-quality care to their patients. In addition to their environmental advantages, concentrators also enhance patient safety. Unlike oxygen cylinders that can pose risks of leakage, combustion, or explosions, oxygen generators operate on electricity and do not involve pressurized oxygen. This eliminates the hazards associated with handling and storing traditional oxygen tanks, making concentrators a safer alternative for both patients and healthcare providers. Furthermore, concentrators are equipped with advanced safety features such as oxygen purity monitors, alarms for low oxygen levels, and power failure backups. These built-in safeguards ensure that patients receive the correct concentration of oxygen at all times, even in the event of power outages or equipment malfunctions. As a result, Medical Oxygen Concentrators provide peace of mind for patients and their caregivers, alleviating concerns about potential risks and emergencies. As the demand for oxygen therapy continues to rise, personalized treatment options become increasingly important. Oxygen generators offer an innovative solution that addresses the unique needs of patients while streamlining healthcare delivery. Their portability, customizability, energy efficiency, and safety features make them a valuable asset in the management of respiratory conditions. Customized oxygen therapy using Medical Oxygen Concentrators has transformed the landscape of respiratory care. These devices offer a multitude of benefits, including personalized treatment, versatile delivery options, energy efficiency, and enhanced patient safety. As healthcare providers and patients embrace this advanced technology, it is evident that oxygen generators are instrumental in optimizing respiratory therapy outcomes and improving the overall well-being of patients. Medical instrumentation has come a long way in recent decades, revolutionizing the field of healthcare and enabling innovative procedures and treatments. One area that has seen significant advancements is tube technology.
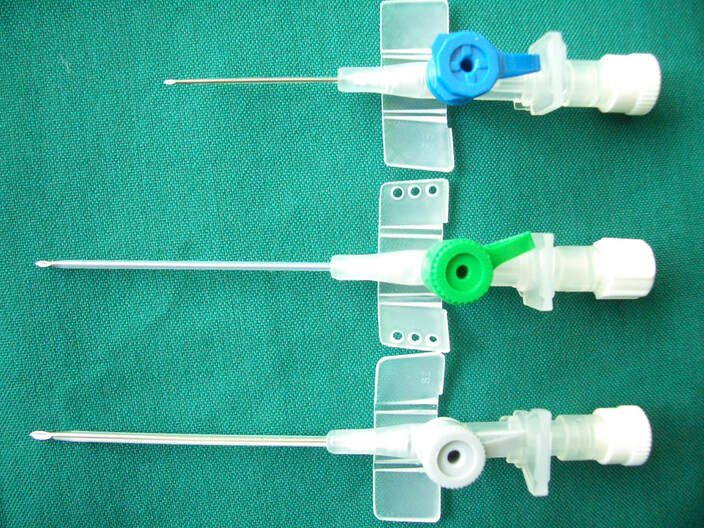
Cannula, slender hollow tubes used for various medical purposes, have evolved to enhance patient care, improve procedural outcomes, and optimize surgical techniques. From their humble beginnings to the cutting-edge designs of today, let's explore the evolution of tube technology and the impact it has had on the medical field. The term "tube" originates from the Latin word "canna," meaning "reed" or "tube." Historically, tube were primarily used for drainage and irrigation purposes. Early tubes were simple, straight tubes made from materials like metal or glass. These basic designs had limited functionality and were prone to causing tissue damage and complications during insertion and removal. Advancements in medical research and technology led to significant improvements in Cannula design and functionality. Modern tubes are constructed from flexible, biocompatible materials like silicone or polyurethane, which minimize tissue trauma and allow for easy insertion and manipulation. These materials are also compatible with various medical applications, including blood transfusion, drug delivery, and tissue sampling. The size and shape of tubes have also evolved over time. Smaller gauge tubes, with diameters as thin as a human hair, have become commonplace. These ultrafine tubes enable less invasive procedures, reducing patient discomfort, scarring, and recovery time. Additionally, curved and tapered tubes have been developed to facilitate precise maneuverability during delicate procedures, such as plastic surgery or ophthalmic interventions. Another significant advancement in tube technology is the incorporation of specialized features to enhance functionality. For example, some Cannula now come equipped with valves or stopcocks that allow for controlled fluid flow or prevent backflow, improving the accuracy and safety of procedures. In certain applications, such as liposuction, tubes may feature suction capabilities to remove unwanted fat deposits effectively. Moreover, the integration of imaging and visualization technologies has revolutionized tube-assisted procedures. The introduction of fiber optics and miniaturized cameras allows surgeons to monitor the progress of a procedure in real-time, providing valuable insights and enhancing precision. This visual feedback helps reduce the risk of complications and ensures accurate placement of the tube in delicate anatomical structures. Advancements in Cannula technology have also given rise to innovative minimally invasive surgical techniques. Procedures like laparoscopy and endoscopy rely heavily on tubes to access internal organs and perform interventions with minimal incisions. These techniques offer numerous benefits over traditional open surgeries, including reduced pain, shorter hospital stays, faster recovery, and improved cosmetic outcomes. In recent years, nanotechnology has begun to make its mark on tube development. Nanocannulas, featuring microscopic dimensions, have shown promise in targeted drug delivery and cellular-level interventions. These ultra-small devices enable precise administration of medication or extraction of cellular samples, opening up new avenues in personalized medicine and regenerative therapies. The evolution of tube technology has had a profound impact on various medical specialties. In cardiology, specialized tubes are used for angioplasty, stent placement, and cardiac catheterization, aiding in the diagnosis and treatment of cardiovascular diseases. In neurosurgery, Cannula assist in intracranial procedures, such as tumor removal or shunt placements. In dermatology, tubes are employed for dermal fillers, reducing the risk of complications and improving patient comfort. Looking ahead, the future of tube technology holds even more promise. Researchers are exploring the integration of sensors and actuators into tubes, allowing for real-time monitoring of physiological parameters and the implementation of robotic-assisted procedures. Furthermore, advancements in 3D printing technology may enable the fabrication of patient-specific tubes, tailored to individual anatomical requirements, further optimizing treatment outcomes. The evolution of tube technology has transformed medical instrumentation, improving patient care and revolutionizing surgical techniques. From basic drainage tubes to sophisticated, minimally invasive devices, Cannulas have come a long way. With ongoing advancements, these slender tubes will continue to play a vital role in the future of healthcare, enabling safer, more precise, and personalized medical interventions. In today's world, personal health and safety have become paramount, and wearing face masks has become an integral part of our daily lives. The importance of choosing the right face mask cannot be overstated. When it comes to ultimate protection, Disposable Face Mask offer convenience, effectiveness, and peace of mind. In this article, we will explore the benefits and features of face masks, highlighting their suitability for daily use.
Superior Protection Disposable masks are designed to provide superior protection against airborne particles, contaminants, and droplets. They act as a physical barrier, preventing the transmission of respiratory droplets that may contain harmful viruses, bacteria, or allergens. High-quality disposable masks are typically made with multiple layers of filtration materials, such as melt-blown fabric, which effectively filters out small particles. They offer a high level of protection for both the wearer and those around them. Hygiene and Convenience One of the key advantages of Disposable Face Mask is their hygienic nature. Each mask is individually packaged, ensuring cleanliness and preventing contamination. This is particularly important for daily use, as it eliminates the need for washing and reusing masks, which can lead to a buildup of bacteria over time. Disposable masks are designed for single-use, making them convenient and hassle-free. After use, simply discard the mask responsibly, reducing the risk of cross-contamination. Comfortable Fit and Breathability Face masks are designed with user comfort in mind. They are lightweight and usually feature adjustable nose clips and ear loops, allowing for a customizable and secure fit. The snug fit not only ensures better protection but also prevents fogging of glasses. Moreover, high-quality disposable masks are engineered to provide adequate breathability, allowing for easy airflow while ensuring efficient filtration. This makes them comfortable to wear for extended periods, even during physical activities. Versatility and Accessibility Disposable Face Masks are available in a wide range of options, catering to different needs and preferences. Whether you require masks for general daily use or specific situations such as travel, healthcare settings, or crowded environments, there is a disposable mask suitable for you. They are also available in various sizes, making them accessible to people of all ages. Additionally, disposable masks are often available in bulk, offering cost-effective solutions for families, businesses, and organizations. Environmental Considerations While the disposable nature of these masks offers convenience and hygiene, it is essential to address environmental concerns. To minimize the ecological impact, it is crucial to choose masks made from eco-friendly materials and dispose of them responsibly. Look for masks that are biodegradable or made from recyclable materials. Many manufacturers are actively working to develop sustainable alternatives to conventional disposable masks, striking a balance between protection and environmental responsibility. In the pursuit of ultimate protection against airborne contaminants, Disposable Face Mask for daily use offer an ideal solution. Their superior protection, convenience, comfortable fit, and breathability make them a reliable choice in various settings. With the wide range of options available, there is a disposable mask to suit every individual's needs. However, it is crucial to remain environmentally conscious and opt for masks made from sustainable materials. By choosing face masks wisely and disposing of them responsibly, we can ensure our health and safety while minimizing our ecological footprint. Stay protected, stay responsible! Sterilization Services are used to remove pathogenic microorganisms from medical or surgical instruments that come into contact with the skin, mucous membranes or sterile tissue. Sterilization helps in removing foreign material such as blood, saliva and other fluids that are left behind after surgery.
Biological indicators are tests used to determine whether a sterilizer is functioning properly and has not lost its effectiveness. This process is conducted on a daily basis in most hospitals. Surgical instruments, needles, and other medical devices that come into contact with sterile body tissues or fluids should be as sterile as possible to prevent the spread of disease. In the US, the Food and Drug Administration (FDA) oversees sterilization techniques used to ensure that medical products are safe for patient use. Disinfection Services help to prevent hospital-acquired infections (HAIs), which are often caused by bacteria, viruses, and fungi. Sterilization Services help to reduce the risk of contamination with toxins and other harmful substances. Disinfection Services involve physical or chemical methods for killing spores, microbes, and viruses that can cause infections in humans. They are used in hospitals & other medical facilities to prevent contamination of surgical instruments and pharmaceutical or healthcare products. Infection prevention guidelines must be adhered to strictly in order to prevent cross-infection from one patient to another. This is why Sterilization Services are needed to ensure that medical devices are free from germs before they are used on a patient. Most surgical and medical devices are made of heat-stable materials and can be sterilized by thermal processes such as steam or ethylene oxide. However, some critical heat or moisture-sensitive items must be sterilized using non-thermal methods. Examples include specialized catheters and endoscopes, as well as some plastic surgery instruments such as scalpels and forceps. Using Sterilization Services allows companies to ensure that their products are properly cleaned and sterilized before being shipped to customers. This eliminates any undesired contaminants that may damage a product or cause health issues to the consumer. This sterilization technique uses high-energy electrons that penetrate matter, ionizing atoms and creating secondary electrons that destroy microorganisms. It is typically used on delicate or heat-sensitive items that can't be sterilized by steam or chemical methods. Disinfection Services are used to decontaminate equipment and supplies that come in contact with patients. Biological indicators are used to validate the lethality of sterilization processes by testing for the presence of spores on finished products. Hospitals often test their sterilizers on a weekly basis. Sterilization Services are used in the food industry to kill harmful organisms that can cause spoilage or infection. It is also used in medical and pharmaceutical industries to ensure that products are free from micro-organisms that can cause diseases. The sterilization process involves heating or radiation to destroy micro-organisms present in food. This method removes yeasts, molds and vegetative bacteria along with spore formers from raw materials like fruits, vegetables, meat and dairy ingredients. It allows manufacturers to store and transport foods safely and extends their shelf-life. Aside from thermal sterilization, chemical sterilization is another popular technique. It uses aggressive chemicals like Hydrofluoric acid and Sodium Hypochlorite to kill micro-organisms. The use of these harsh chemicals requires special protection measures to prevent contamination of surrounding areas and equipment. Specialized product trays like those designed and manufactured by NGS industrial are often required to hold instruments or items during the chemical sterilization process. The medical device industry uses a variety of physical, chemical, radiation, and ethylene oxide (EtO) gas sterilization methods to ensure that the products are sterile for patient use. These methods require rigorous validation, routine process control, and compliance with voluntary consensus standards administered by the International Organization for Standardization. The emergence of multidrug-resistant (MDR) bacteria and their biofilms poses a serious threat to health care facilities. Infections resulting from contaminated reusable medical devices can be devastating to immunocompromised patients. MDR pathogens are particularly prone to colonize medical devices with flexible accessories that can easily be re-contaminated between patients. In the world of healthcare, innovation is constantly evolving to enhance patient experience and improve treatment outcomes. One such advancement that has gained significant attention is Transdermal Skin Patches.
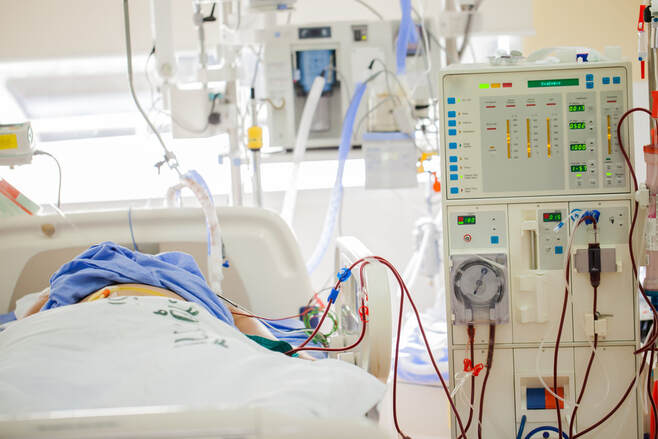
These patches have revolutionized the way certain medications are delivered, offering patients a convenient and effective alternative to traditional oral or injectable forms of therapy. By providing a controlled and continuous release of medication through the skin, transdermal patches have empowered patients, allowing them to take control of their health and receive care on their terms. Transdermal patches are designed to adhere to the surface of the skin, delivering medication directly into the bloodstream. This method bypasses the digestive system, avoiding the need for oral ingestion and the potential breakdown of the drug by stomach acids or liver metabolism. By delivering medication directly into the bloodstream, transdermal patches ensure a consistent and steady release of the drug over an extended period, providing more predictable and controlled therapy. One of the key advantages of Transdermal Skin Patches is their convenience. Unlike oral medications that require frequent dosing or injections that may be invasive and painful, patches can be easily applied and worn discreetly under clothing. This enables patients to maintain their regular daily routines without interruption, allowing them to focus on their work, family, or leisure activities while receiving the necessary treatment. Furthermore, transdermal patches eliminate the need for multiple daily administrations, reducing the risk of missed doses and improving patient adherence to the prescribed therapy. Another significant benefit of Transdermal Skin Patches is the potential for improved drug absorption and bioavailability. Some medications are poorly absorbed when taken orally due to factors such as low solubility or susceptibility to enzymatic degradation. Transdermal delivery bypasses these issues, allowing drugs to be absorbed directly into the bloodstream. This can lead to improved therapeutic outcomes and reduced side effects, as the drug is delivered in its active form without being altered by the digestive system. Transdermal Skin Patches have proven particularly valuable in the management of chronic conditions such as pain, hormone imbalances, and cardiovascular diseases. Pain relief patches, for example, provide localized analgesia by delivering medications like opioids or nonsteroidal anti-inflammatory drugs (NSAIDs) directly to the affected area. Hormone patches are used to balance hormone levels in conditions like menopause or hypothyroidism, providing a steady release of hormones that can alleviate symptoms and improve quality of life. Additionally, cardiovascular patches can deliver medications for conditions like high blood pressure or angina, ensuring a continuous and controlled release of the drug for optimal efficacy. Furthermore, transdermal patches can offer a safer alternative for certain patient populations. For individuals who have difficulty swallowing pills or may have gastrointestinal disorders that affect oral absorption, patches provide a viable solution. In addition, patches eliminate the need for injections, reducing the risk of needlestick injuries and associated complications. This makes transdermal patches particularly valuable for pediatric patients, elderly individuals, and those with needle phobia or limited dexterity. Transdermal Skin Patches have revolutionized the way medications are delivered, empowering patients with convenient care. By offering a controlled and continuous release of medication, these patches ensure consistent therapy and improved treatment outcomes. Their convenience, ease of use, and potential for improved drug absorption make them an attractive option for patients and healthcare providers alike. As technology continues to advance, we can expect further advancements in transdermal delivery systems, providing even greater opportunities for patients to take control of their health and well-being. Innovative Solutions for Kidney Health: Next-Generation Kidney Dialysis Equipment for Children6/28/2023 Kidney disease is a serious health concern that affects millions of people worldwide, including children. For children with kidney failure, dialysis becomes a crucial lifeline, allowing them to survive while awaiting a kidney transplant. However, traditional dialysis equipment can be challenging for young patients, causing discomfort and hindering their quality of life.
To address this issue, researchers and medical device manufacturers have been working tirelessly to develop next-generation Kidney Dialysis Equipment specifically designed for children. These innovative solutions aim to improve the overall experience of pediatric patients and enhance their long-term kidney health. One of the key areas of focus in developing next-generation kidney dialysis devices for children is to make the treatment process less intimidating and more child-friendly. Traditional dialysis machines are large, noisy, and can be overwhelming for young patients. The new equipment being developed incorporates colorful designs, friendly shapes, and interactive features to create a more welcoming and comforting environment. The aim is to reduce anxiety and fear in children undergoing dialysis, making the experience less traumatic and more manageable for both the child and their parents or caregivers. Another important aspect of next-generation Kidney Dialysis Equipment for children is its size and portability. Traditional dialysis machines are typically bulky and immobile, limiting the child's mobility and ability to engage in normal daily activities. The new equipment is being designed to be compact, lightweight, and portable, allowing children to move around more freely and continue with their education, hobbies, and social interactions. This improved mobility can significantly enhance the child's overall well-being and quality of life, reducing the sense of confinement often associated with dialysis treatment. In addition to the physical design enhancements, the next-generation Kidney Dialysis Equipment for children also focuses on improving the efficiency and effectiveness of the treatment itself. Researchers are exploring advanced filtration technologies that optimize the removal of waste products and toxins from the blood while minimizing the loss of essential nutrients. This not only enhances the efficacy of dialysis but also reduces the time required for each session. Shorter treatment times allow children to spend more time engaging in activities they enjoy, promoting a sense of normalcy and reducing the disruption caused by dialysis. Moreover, the development of next-generation Kidney Dialysis Equipment for children includes the integration of digital technologies. Connected devices and smart sensors enable real-time monitoring of vital signs, fluid balance, and treatment parameters, providing healthcare professionals with valuable insights and allowing for timely adjustments to the treatment plan. These digital advancements help ensure a more precise and personalized dialysis experience for each child, improving treatment outcomes and reducing the risk of complications. Furthermore, advancements in telemedicine and remote patient monitoring have the potential to revolutionize pediatric kidney dialysis. By leveraging telehealth solutions, medical professionals can remotely monitor a child's dialysis treatment and provide support from a distance. This eliminates the need for frequent hospital visits, reduces travel-related stress, and enables children to receive the necessary care in the comfort of their own homes. Remote monitoring also facilitates regular communication between the medical team and the child's family, promoting greater engagement and shared decision-making. The development of next-generation Kidney Dialysis Equipment for children is a significant step forward in improving the quality of life and long-term kidney health for pediatric patients. These innovative solutions aim to make dialysis treatment less intimidating, more child-friendly, and technologically advanced. By incorporating appealing designs, portability, advanced filtration techniques, and digital technologies, these new devices offer children a more comfortable, efficient, and personalized dialysis experience. As research and development in this field continue, we can look forward to further advancements that will revolutionize kidney health for children and provide them with brighter and healthier futures. The field of wound care management has seen significant advancements in recent years, revolutionizing the way healthcare professionals approach the treatment of complex wounds. These advancements have led to improved patient outcomes, faster healing times, and a reduction in complications. In this comprehensive guide, we will explore the latest advancements in Advanced Wound Care Management, highlighting the innovative techniques, therapies, and technologies that are reshaping the landscape of wound care.
Advanced Dressings and Topical Agents One of the key areas of advancement in wound care management is the development of advanced dressings and topical agents. Traditional wound dressings have been replaced with more sophisticated options that promote faster healing and provide an optimal wound environment. For instance, there are now dressings infused with antimicrobial agents, which help prevent infection and promote a sterile healing environment. Additionally, bioactive dressings that contain growth factors, such as platelet-derived growth factor (PDGF) and epidermal growth factor (EGF), have shown promising results in stimulating tissue regeneration and accelerating wound closure. Negative Pressure Wound Therapy (NPWT) Negative Pressure Wound Therapy (NPWT) has emerged as a game-changer in Advanced Wound Care Management. NPWT involves the application of controlled negative pressure to the wound bed through a specialized dressing. This technique enhances wound healing by removing excess fluid, promoting blood flow, reducing edema, and stimulating the formation of granulation tissue. NPWT has proven particularly effective in the management of chronic, non-healing wounds, such as pressure ulcers, diabetic foot ulcers, and venous leg ulcers. Hyperbaric Oxygen Therapy (HBOT) Hyperbaric Oxygen Therapy (HBOT) is another groundbreaking advancement in wound care management. This therapy involves the administration of 100% pure oxygen at a higher atmospheric pressure inside a hyperbaric chamber. The increased oxygen concentration and pressure facilitate the delivery of oxygen to tissues, promoting angiogenesis, enhancing the antimicrobial activity, and stimulating collagen synthesis. HBOT has shown remarkable results in the treatment of complex wounds, including diabetic ulcers, radiation-induced tissue damage, and crush injuries. Biologic and Regenerative Therapies Biologic and regenerative therapies have revolutionized the field of Advanced Wound Care Management by harnessing the body's natural healing abilities. These therapies involve the application of living cells, growth factors, and other biological agents to promote wound healing. For example, autologous platelet-rich plasma (PRP) derived from the patient's own blood contains high concentrations of growth factors that can accelerate wound healing. Similarly, stem cell therapy has shown promise in regenerating damaged tissues and promoting wound closure. These regenerative therapies hold immense potential for treating chronic wounds and significantly improving healing outcomes. Advanced Imaging and Monitoring Technologies Advancements in imaging and monitoring technologies have also played a crucial role in wound care management. High-resolution imaging techniques, such as ultrasound, infrared imaging, and optical coherence tomography, allow healthcare professionals to visualize wound depth, tissue perfusion, and the presence of infection. These imaging modalities aid in accurate wound assessment and help guide treatment decisions. Moreover, remote monitoring systems and smart dressings equipped with sensors can provide real-time data on wound status, including temperature, moisture levels, and bacterial load. This enables healthcare providers to intervene promptly and make informed decisions based on objective measurements. The advancements in Advanced Wound Care Management have transformed the way healthcare professionals approach the treatment of complex wounds. From advanced dressings and topical agents to innovative therapies and cutting-edge imaging technologies, the field of wound care has witnessed remarkable progress. These advancements have led to improved healing outcomes, reduced complications, and enhanced quality of life for patients. As research continues and technology advances, we can expect further breakthroughs in wound care management, ultimately Electrosurgery in the Digital Era: Harnessing the Power of Advanced Electrosurgical Devices6/28/2023 Electrosurgery has long been a crucial technique in modern medicine, enabling surgeons to perform precise and efficient procedures. Over the years, advancements in technology have transformed Electrosurgical Devices, taking them to new heights in the digital era. With the advent of advanced electrosurgical equipments, healthcare professionals now have access to powerful tools that offer improved precision, control, and patient outcomes.
One of the key advancements in electrosurgery is the integration of digital technology into surgical devices. Digital electrosurgical units (ESUs) have revolutionized the field by offering enhanced safety features, improved user interfaces, and increased procedural efficiency. These devices incorporate sophisticated microprocessors and sensors that monitor and control the flow of electrical energy, ensuring optimal performance and minimizing the risk of complications. One of the notable features of advanced electrosurgical equipments is their ability to deliver different modes of energy, such as monopolar and bipolar, with precision and customization. Monopolar electrosurgery involves the use of a single active electrode, while bipolar electrosurgery utilizes two electrodes. The digital era has witnessed the development of devices that allow surgeons to seamlessly switch between modes, catering to the specific needs of each procedure. This versatility improves the surgeon's ability to perform delicate surgeries while minimizing thermal damage to surrounding tissues. Furthermore, the integration of digital technology has led to the development of Electrosurgical Devices with advanced energy management systems. These systems monitor the tissue impedance during surgery and automatically adjust the energy delivery to maintain optimal cutting and coagulation effects. By providing real-time feedback, these devices enhance the surgeon's ability to achieve precise tissue dissection and hemostasis, resulting in improved surgical outcomes and reduced operative times. Another significant advancement in electrosurgical equipments is the integration of advanced imaging technologies. Digital electrosurgical equipments can now be equipped with high-definition cameras and endoscopic systems, allowing surgeons to visualize the surgical site with exceptional clarity. This integration facilitates minimally invasive procedures, as surgeons can navigate complex anatomical structures and perform precise tissue manipulation with enhanced visualization. The combination of electrosurgery and advanced imaging techniques has opened up new possibilities for procedures that were previously considered challenging or high-risk. Moreover, the digital era has witnessed the development of Electrosurgical Devices with improved ergonomic designs. Surgeons can now benefit from lightweight, user-friendly devices that offer enhanced maneuverability and control. These advancements reduce fatigue and improve precision during lengthy procedures, leading to better surgical outcomes and increased patient safety. The digital era has also paved the way for the integration of Electrosurgical Devices with data management systems and electronic health records (EHRs). Surgeons can now seamlessly document surgical parameters, energy settings, and patient information, allowing for better documentation and analysis of procedures. This integration not only enhances surgical workflow but also enables the collection of valuable data for research, quality improvement, and future advancements in electrosurgery. However, it is essential to recognize that with the power and capabilities of advanced Electrosurgical Devices come the need for proper training and ongoing education. Surgeons and healthcare professionals must stay updated with the latest advancements and techniques to maximize the benefits and ensure patient safety. Manufacturers and regulatory bodies play a vital role in providing comprehensive training programs and guidelines for the safe and effective use of advanced electrosurgical equipments. The digital era has ushered in a new era of electrosurgery, empowering surgeons with advanced devices that offer precision, control, and improved patient outcomes. The integration of digital technology, advanced energy management systems, imaging technologies, and ergonomic designs has revolutionized the field, allowing for more precise procedures and reduced risks. As we continue to embrace the power of advanced Electrosurgical Devices, it is crucial to prioritize training, education, and safety to harness their full potential and shape the future of surgical interventions. |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
July 2023
Categories
All
|








 RSS Feed
RSS Feed
